Hi everyone, welcome to our fourth guest blog post. Today we will have Dr. Ashley Martinez (PharmD, PhD) from the University of Kentucky summarizing her recent PhD dissertation – and discussing medication appropriateness measurement tools to meaningfully identify potentially inappropriate medications.
Meaningful Measurement Matters!
If you’ve been following the blog, you’ll recall the recent post exploring a study which found that less than one-quarter of health professional students were familiar with the term “deprescribing.” While this lack of familiarity may be shocking to those of us who have poured our hearts and souls into improving appropriate medication use, we should remember that our field is a relatively new one.
A Little History
It was a mere 30 years ago that Dr. Mark Beers led a panel of geriatric experts to develop a list of 30 therapeutic classes and medications that should be avoided in older adults who resided in nursing homes. The Beers Criteria has since become one of the most often cited medication appropriateness assessment tools and is recommended to guide prescribing decisions in all older adults.
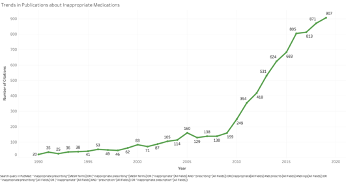
Over the next 20 years, nearly 2,000 research articles would be indexed in PubMed about potentially inappropriate medication (PIM) use. But the popularity of this newfound field of research did not stop there. In the decade since 2010, nearly 6,500 more articles have been published – and researchers have developed more than 70 different medication appropriateness assessment tools!
The Time is Now
In an ideal world, this influx of data would lead to evidence that would directly translate to patient care. Unfortunately, a recent systematic review found that only about one-third of published studies investigating potentially inappropriate medication use attempt to link it with any clinical outcome.
While it’s exciting to be in this world of deprescribing research (especially as a newly minted PhD :D), it’s also disappointing to me as a pharmacist that patients may not be reaping the benefit of all this hard work. What good can come of the more than 70 medication appropriateness assessment tools if we aren’t certain that they can measure medication use in a way that is clinically meaningful for patients? What can “PIM use” even mean, if there are 70 different definitions?
It was this question that led me down the path to my doctoral dissertation. Fortunately, I believe the field is still new enough to refocus our efforts toward finding a meaningful measure of PIM use. Because of my clinical interest in memory problems, I chose to investigate whether there were published medication appropriateness assessment tools that meaningfully identified PIM use as it related to cognitive outcomes.
Ultimately, my goal is to provide evidence to clinicians, researchers, and institutions that now is the time to take a collective moment to figure out what we’re measuring. Only then will we be able to move forward to improve the lives of our older adult fellow citizens.
My work
My dissertation begins with a review of the published medication appropriateness assessment tools that have been validated for any cognitive outcome. While I’ll spare the gory details for an upcoming publication, spoiler alert: there are only six. Yes, you read that right: only SIX out of SEVENTY-SIX medication appropriateness assessment tools have ever been studied for their ability to identify PIM use that may be related to cognitive outcomes. In case my utter shock is not conveyed through your computer screen, I’ll just remind you that Alzheimer’s disease and related dementias are the fifth leading cause of death globally and the only one out of the top ten medical conditions without an effective treatment or cure! What an opportunity for us to reduce the impact of dementias by deprescribing medications that may be adding fuel to this fire.
The next section of my dissertation compares prevalence estimates of PIM use using various tools, and unsurprisingly concludes that the different tools lead to starkly different estimates of PIM use. This section highlights one important consequence of using so many different PIM assessment tools: we cannot convey the extent of our exposure if we cannot decide on a meaningful measurement of it. My studies show prevalence of PIM use from less than 1% to nearly 80%, depending on the tool used.
I then move on to investigating whether any published tool identifies PIM use that is meaningfully connected to cognitive impairment or decline. There are currently 17 published studies that have attempted to validate various PIM identification tools to cognitive outcomes. Each uses a similar study design and statistical analysis. In my dissertation, I use various aspects of the causal inference framework to attempt to answer more clinically relevant research questions regarding the relationship between these tools and cognitive outcomes. I’m looking forward to sharing the results with everyone in the near future.
Moving Forward
Without a clear consensus on how to measure PIM use to target cognitive outcomes, systematic reviews will continue to conclude that “more evidence is needed,” before we can reach a conclusion about the impact of PIM use on health. Of course, in order to reach such a consensus, investigators need support from their institutions and government leaders. As I show in my dissertation, implementation of national and local initiatives to validate PIM identification tools to health outcomes can have sweeping positive effects.
All stakeholders in this important area have a role to play in furthering the study of how PIM use is impacting cognition in older adults. We must also take responsibility to pause and clearly define the exposure of interest, or our progress may never bear its fruit.
I’m looking forward to publishing the studies I conducted, so keep an eye out for those in the future. You can follow me on Twitter (@ashleyirene09) – I’d love to hear from you! For anyone interested in this area of deprescribing for cognitive health, I’d also recommend following my mentors (and rockstars, without whom my dissertation would not be here!), Dr. Daniela Moga (@epidmoga) and Dr. Erin Abner (@ErinAbnerPhD).
The deprescribing blog is hosted by pharmacists and PhD students, Carina Lundby and Wade Thompson. We hope to be your new best deprescribing friends and supply you with deprescribing content and analysis on a biweekly basis. Please reach out to us if you have any questions or comments, or would like to contribute.
carina.lundby.olesen@rsyd.dk (Twitter: @CarinaLundby)
wthompson@health.sdu.dk (Twitter: @wadddee)